From Wikipedia, the free encyclopedia
Classification & external resources
ICD-10
M48.0
ICD-9
723-724
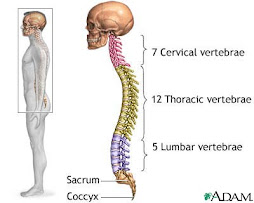
Spinal stenosis is a medical condition in which the spinal canal narrows and compresses the spinal cord and nerves. This is usually due to the natural process of spinal degeneration that occurs with aging. It can also sometimes be caused by spinal disc herniation, osteoporosis, or a tumour. Spinal stenosis may affect the cervical spine, the lumbar spine or both. Lumbar spinal stenosis results in low back pain as well as pain or abnormal sensations in the legs.
Cervical spinal stenosis
The main causes of cervical spinal stenosis (CSS) include cervical spondylosis, diffuse idiopathic skeletal hyperostosis (DISH), or calcification of the posterior longitudinal ligament.
CSS is more common in males than females, and is mainly found in the 40-60 year age group.
Signs of CSS include spastic gait; upper extremity numbness; upper extremity, lower extremity weakness or both; radicular pain in the upper limb; sphincter disturbances; muscle wasting; sensory deficits; and reflex abnormalities.
Diagnosis
The best diagnostic and investigative tool is magnetic resonance imaging (MRI), while computed tomograghy (CT) is somewhat useful if MRI is unavailable. However, spinal stenosis can be found in asymptomatic patients.[1][2][3]
Treatment
If the problem is mild, treatment may be as simple as physical therapy and the use of a cervical collar. If severe, treatments include laminectomy, hemilaminectomy, or decompression.
Lumbar spinal stenosis
The main causes of lumbar spinal stenosis (LSS) include hypertrophy of the facet joints or osteoarthritis; spondylolisthesis; diffuse idiopathic skeletal hyperostosis (DISH); and degenerative disc disease.
Usually, this condition occurs after the age of 50, and both genders are equally affected.
Signs of LSS include neurogenic intermittent claudication that causes leg pain, weakness, tingling and loss of deep tendon reflexes. Many of these leg symptoms are referred to as sciatica. Low back pain may or may not be present. With lumbar spinal stenosis, the patient's pain usually is worse while walking and will feel better after sitting down. The patient is usually more comfortable while leaning forward, such as walking while leaning on a shopping cart. On the other hand, pain is worse with extension of the back at the hips, which is why patients prefer to lean forward or to sit down, as these actions flex the body at the hip. This is also why patients complain of increased pain walking downhill as opposed to uphill.
Diagnosis
As with CSS, MRI is the best imaging procedure, though unlike with CSS, CT may be somewhat useful, and can be used if MRI is unavailable.
Treatment
Treatment includes weight loss, and activity modification, such as using a walker to promote a certain posture. Epidural steroid injections may also help relieve the leg pain.
If the symptoms are more severe, a laminectomy or foraminotomy may be indicated to take pressure off the spinal nerve.
Surgical laminectomy
Regarding indications for laminectomy, a complicated, nonrandomized analysis of a randomized controlled trial of laminectomy[4], in patients with:
"neurogenic claudication or radicular leg pain with associated neurologic signs, spinal stenosis shown on cross-sectional imaging, and degenerative spondylolisthesis shown on lateral radiographs obtained with the patient in a standing position. The patients had had persistent symptoms for at least 12 weeks and had been confirmed as surgical candidates by their physicians. Patients with adjacent levels of stenosis were eligible; patients with spondylolysis and isthmic spondylolisthesis were not."
found that patients:
"treated surgically showed substantially greater improvement in pain and function during a period of 2 years than patients treated nonsurgically."
New surgical developments
Recent developments include several new implants used in surgery to treat the symptoms of spinal stenosis, while preserving as much normal motion in the spine as possible. The only FDA approved non-fusion treatment is the X STOP, by St. Francis Medical Techologies, Inc. which works via indirect decompression, called Interspinous Process Decompression [1](IPD) Some other IPD technologies that are still being studied include the Wallis implant, by Aboott Spine , the DIAM by Medtronic and the Coflex by Paradigm Spine, .[5] Other implant systems being studied include the Dynesys by Zimmer, the Stabilimax by Applied Spine, the TFAS by Archus Orthopedics and the Anatomic Facet Replacement System, by Facet Solutions.
One recent implant system that was being studied in the US reportedly has problems that ended its enrollment, the TOPS implant by Impliant. This was reported [2]by an investor in Impliant, Elron Ltd.
Also recently, Medtronic's non-fusion implant was recalled officially in the United Kingdom [3], though in the US the device has been withdrawn from surgeons but MDT has not issued a recall, probably due to the way inventory is handled rather than a difference in the product sold in the US vs. the UK.
External links
Spinal Stenosis.org
Spinal Stenosis - Information for Patients
Lumbar Spinal Stenosis
Cervical Disorders - Spinal Stenosis and Disc Herniation
References
^ Teresi LM, Lufkin RB, Reicher MA, et al (1987). "Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging". Radiology 164 (1): 83-8. PMID 3588931.
^ Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S (1990). "Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation". The Journal of bone and joint surgery. American volume 72 (8): 1178-84. PMID 2398088.
^ Ernst CW, Stadnik TW, Peeters E, Breucq C, Osteaux MJ (2005). "Prevalence of annular tears and disc herniations on MR images of the cervical spine in symptom free volunteers". European journal of radiology 55 (3): 409-14. doi:10.1016/j.ejrad.2004.11.003. PMID 16129249.
^ Weinstein JN, Lurie JD, Tosteson TD, et al (2007). "Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis". N. Engl. J. Med. 356 (22): 2257-70. doi:10.1056/NEJMoa070302. PMID 17538085.
^ B. Stromqvist (2006). Lumbar Spinal Stenosis - Striving for Less Invasive Surgery.
[hide]
v • d • eDiseases of the musculoskeletal system and connective tissue (M, 710-739)
Arthropathies
Arthritis (Septic arthritis, Reactive arthritis, Rheumatoid arthritis, Psoriatic arthritis, Felty's syndrome, Juvenile idiopathic arthritis, Still's disease) - crystal (Gout, Chondrocalcinosis) - Osteoarthritis (Heberden's node, Bouchard's nodes)
acquired deformities of fingers and toes (Boutonniere deformity, Bunion, Hallux rigidus, Hallux varus, Hammer toe) - other acquired deformities of limbs (Valgus deformity, Varus deformity, Wrist drop, Foot drop, Flat feet, Club foot, Unequal leg length, Winged scapula)
patella (Luxating patella, Chondromalacia patellae)Protrusio acetabuli - Hemarthrosis - Arthralgia - Osteophyte
Systemic connectivetissue disorders
Polyarteritis nodosa - Churg-Strauss syndrome - Kawasaki disease - Hypersensitivity vasculitis - Goodpasture's syndrome - Wegener's granulomatosis - Arteritis (Takayasu's arteritis, Temporal arteritis) - Microscopic polyangiitis - Systemic lupus erythematosus (Drug-induced) - Dermatomyositis (Juvenile dermatomyositis) - Polymyositis - Scleroderma - Sjögren's syndrome - Behçet's disease - Polymyalgia rheumatica - Eosinophilic fasciitis - Hypermobility
Dorsopathies
Kyphosis - Lordosis - Scoliosis - Scheuermann's disease - Spondylolysis - Torticollis - Spondylolisthesis - Spondylopathies (Ankylosing spondylitis, Spondylosis, Spinal stenosis) - Schmorl's nodes - Degenerative disc disease - Coccydynia - Back pain (Radiculopathy, Neck pain, Sciatica, Low back pain)
Soft tissue disorders
muscle: Myositis - Myositis ossificans (Fibrodysplasia ossificans progressiva)
synovium and tendon: Synovitis/Tenosynovitis (Calcific tendinitis, Stenosing tenosynovitis, Trigger finger, DeQuervain's syndrome) - Irritable hip - Ganglion cyst
bursa: bursitis (Olecranon, Prepatellar, Trochanteric) - Baker's cyst
fibroblastic disorders (Dupuytren's contracture, Plantar fasciitis, Nodular fasciitis, Necrotizing fasciitis, Fasciitis, Fibromatosis)
shoulder lesions: Adhesive capsulitis - Rotator cuff tear - Subacromial bursitis
enthesis: enthesopathies (Iliotibial band syndrome, Achilles tendinitis, Patellar tendinitis, Golfer's elbow, Tennis elbow, Metatarsalgia, Bone spur, Tendinitis)other, NEC: Muscle weakness - Rheumatism - Myalgia - Neuralgia - Neuritis - Panniculitis - Fibromyalgia
Osteopathies
disorders of bone density and structure: Osteoporosis - Osteomalacia - continuity of bone (Pseudarthrosis, Stress fracture) - Monostotic fibrous dysplasia - Skeletal fluorosis - Aneurysmal bone cyst - Hyperostosis - OsteosclerosisOsteomyelitis - Avascular necrosis - Paget's disease of bone - Algoneurodystrophy - Osteolysis - Infantile cortical hyperostosis
Chondropathies
Juvenile osteochondrosis (Legg-Calvé-Perthes syndrome, Osgood-Schlatter disease, Köhler disease, Sever's disease) - Osteochondritis - Tietze's syndrome
See also congenital conditions (Q65-Q79, 754-756)
Retrieved from "http://en.wikipedia.org/wiki/Spinal_stenosis"
Categories: Skeletal disorders
Degenerative disc disease
From Wikipedia, the free encyclopedia
Classification & external resources
ICD-9
722.6
DiseasesDB
6861
Degeneration of the intervertebral disc, which is often called "degenerative disc disease" (DDD) of the spine,DDD is in fact a condition that can be painful and can greatly affect the quality of one's life. While disc degeneration is a normal part of aging and for most people is not a problem, for certain individuals a degenerated disc can cause severe constant chronic pain.
Causes
Trauma micro or macro as a simple lifting accident is the most common cause of disc degeneration. After trauma the discs in the spine dehydrate, or dry out, and lose their ability to act as shock absorbers between the vertebrae. There is minimal blood supply to the discs so they lack the ability to heal or repair themselves.
Symptoms
With symptomatic degenerative disc disease, chronic low back pain sometimes radiates to the hips, or there is an aching pain in the buttocks or thighs while walking; sporadic tingling or weakness through the knees may also be evident. Similar pain may be felt or may increase while sitting, bending, lifting, and twisting.
Understanding disc pain
After an injury, some discs become painful because of inflammation. Some people have nerve endings that penetrate more deeply into the annulus fibrosus, or outer layer of the disc, than others, making the disc more susceptible to becoming a source of pain. The scientific community have the opinion that the healing process involved in the repair of trauma to the outer annulous results in the innervation of the resultant scar tissue, and subsequent pain in the disc, as these nerves become inflamed by nucleous pulposus material. Degenerative disc disease can lead to a chronic debilitating condition and can have a serious negative impact on a person's quality of life. When pain from degenerative disc disease is severe, traditional nonoperative treatment is often ineffective.
Treatment options
Often, degenerative disc disease can be successfully treated without surgery. One or a combination of treatments such as Physical therapy, osteopathy, anti-inflammatory medications such as nonsteroidal anti-inflammatory drugs, chiropractic treatments, or spinal injections often provide adequate relief of these troubling symptoms.
Surgery may be recommended if the conservative treatment options do not provide relief within 2 to 3 months. If leg or back pain limits normal activity, if there is weakness or numbness in the legs, if it is difficult to walk or stand, or if medication or physical therapy are ineffective, surgery may be necessary, most often spinal fusion. There are many surgical options for the treatment of degenerative disc disease. The most common surgical treatmets include:[1]
- Anterior Cervical Discectomy and Fusion: A procedure that reaches the cervical spine (neck) through a small incision in the front of the neck. The intervertebral disc is removed and replaced with a small plug of bone or other graft substitute, and in time, that will fuse the vertebrae.
- Cervical Corpectomy: A procedure that removes a portion of the vertebra and adjacent intervertebral discs to allow for decompression of the cervical spinal cord and spinal nerves. A bone graft, and in some cases a metal plate and screws, is used to stabilize the spine.
- Facetectomy: A procedure that removes a part of the facet (a bony structure in the spinal canal) to increase the space.
- Foraminotomy: A procedure that enlarges the foramen (the area where the nerve roots exit the spinal canal) to increase the size of the nerve pathway. This surgery can be done alone or with a laminotomy.
- Laminoplasty: A procedure that reaches the cervical spine (neck) from the back of the neck. The spinal canal is then reconstructed to make more room for the spinal cord.
- Laminotomy: A procedure that removes only a small portion of the lamina (a part of the vertebra) to relieve pressure on the nerve roots.
- Micro-discectomy: A procedure that removes a disc through a very small incision using a microscope.
- Spinal Laminectomy: A procedure for treating spinal stenosis by relieving pressure on the spinal cord. A part of the lamina (a part of the vertebra) is removed or trimmed to widen the spinal canal and create more space for the spinal nerves.
New treatments are emerging that are still in the beginning clinical trial phases. Glucosamine injections are thought to offer some pain relief for degenerative discs at best, and at worst, do nothing while also not affecting more aggressive treatment options. Artificial disc replacement is viewed cautiously as a possible alternative to fusion in carefully selected patients. Adult stem cell therapies for disc regeneration are in their infancy. [1] . Mesechymal stem cell therapy trials for knife-less fusion of vertebrae are now beginning in the US as well [2]. Gene therapy, growth factor injections, and a variety of stabilization devices are also on the horizon.
References
^ Degenerative Disc Disease - When Surgery Is Needed. Retrieved on 2007-06-26.
v • d • eDiseases of the musculoskeletal system and connective tissue (M, 710-739)
Arthropathies
Arthritis (Septic arthritis, Reactive arthritis, Rheumatoid arthritis, Psoriatic arthritis, Felty's syndrome, Juvenile idiopathic arthritis, Still's disease) - crystal (Gout, Chondrocalcinosis) - Osteoarthritis (Heberden's node, Bouchard's nodes)
acquired deformities of fingers and toes (Boutonniere deformity, Bunion, Hallux rigidus, Hallux varus, Hammer toe) - other acquired deformities of limbs (Valgus deformity, Varus deformity, Wrist drop, Foot drop, Flat feet, Club foot, Unequal leg length, Winged scapula)
patella (Luxating patella, Chondromalacia patellae)Protrusio acetabuli - Hemarthrosis - Arthralgia - Osteophyte
Systemic connectivetissue disorders
Polyarteritis nodosa - Churg-Strauss syndrome - Kawasaki disease - Hypersensitivity vasculitis - Goodpasture's syndrome - Wegener's granulomatosis - Arteritis (Takayasu's arteritis, Temporal arteritis) - Microscopic polyangiitis - Systemic lupus erythematosus (Drug-induced) - Dermatomyositis (Juvenile dermatomyositis) - Polymyositis - Scleroderma - Sjögren's syndrome - Behçet's disease - Polymyalgia rheumatica - Eosinophilic fasciitis - Hypermobility
Dorsopathies
Kyphosis - Lordosis - Scoliosis - Scheuermann's disease - Spondylolysis - Torticollis - Spondylolisthesis - Spondylopathies (Ankylosing spondylitis, Spondylosis, Spinal stenosis) - Schmorl's nodes - Degenerative disc disease - Coccydynia - Back pain (Radiculopathy, Neck pain, Sciatica, Low back pain)
Soft tissue disorders
muscle: Myositis - Myositis ossificans (Fibrodysplasia ossificans progressiva)
synovium and tendon: Synovitis/Tenosynovitis (Calcific tendinitis, Stenosing tenosynovitis, Trigger finger, DeQuervain's syndrome) - Irritable hip - Ganglion cyst
bursa: bursitis (Olecranon, Prepatellar, Trochanteric) - Baker's cyst
fibroblastic disorders (Dupuytren's contracture, Plantar fasciitis, Nodular fasciitis, Necrotizing fasciitis, Fasciitis, Fibromatosis)
shoulder lesions: Adhesive capsulitis - Rotator cuff tear - Subacromial bursitis
enthesis: enthesopathies (Iliotibial band syndrome, Achilles tendinitis, Patellar tendinitis, Golfer's elbow, Tennis elbow, Metatarsalgia, Bone spur, Tendinitis)other, NEC: Muscle weakness - Rheumatism - Myalgia - Neuralgia - Neuritis - Panniculitis - Fibromyalgia
Osteopathies
disorders of bone density and structure: Osteoporosis - Osteomalacia - continuity of bone (Pseudarthrosis, Stress fracture) - Monostotic fibrous dysplasia - Skeletal fluorosis - Aneurysmal bone cyst - Hyperostosis - OsteosclerosisOsteomyelitis - Avascular necrosis - Paget's disease of bone - Algoneurodystrophy - Osteolysis - Infantile cortical hyperostosis
Chondropathies
Juvenile osteochondrosis (Legg-Calvé-Perthes syndrome, Osgood-Schlatter disease, Köhler disease, Sever's disease) - Osteochondritis - Tietze's syndrome
See also congenital conditions (Q65-Q79, 754-756)
Retrieved from "http://en.wikipedia.org/wiki/Degenerative_disc_disease"
References
^ Degenerative Disc Disease - When Surgery Is Needed. Retrieved on 2007-06-26.
v • d • eDiseases of the musculoskeletal system and connective tissue (M, 710-739)
Arthropathies
Arthritis (Septic arthritis, Reactive arthritis, Rheumatoid arthritis, Psoriatic arthritis, Felty's syndrome, Juvenile idiopathic arthritis, Still's disease) - crystal (Gout, Chondrocalcinosis) - Osteoarthritis (Heberden's node, Bouchard's nodes)
acquired deformities of fingers and toes (Boutonniere deformity, Bunion, Hallux rigidus, Hallux varus, Hammer toe) - other acquired deformities of limbs (Valgus deformity, Varus deformity, Wrist drop, Foot drop, Flat feet, Club foot, Unequal leg length, Winged scapula)
patella (Luxating patella, Chondromalacia patellae)Protrusio acetabuli - Hemarthrosis - Arthralgia - Osteophyte
Systemic connectivetissue disorders
Polyarteritis nodosa - Churg-Strauss syndrome - Kawasaki disease - Hypersensitivity vasculitis - Goodpasture's syndrome - Wegener's granulomatosis - Arteritis (Takayasu's arteritis, Temporal arteritis) - Microscopic polyangiitis - Systemic lupus erythematosus (Drug-induced) - Dermatomyositis (Juvenile dermatomyositis) - Polymyositis - Scleroderma - Sjögren's syndrome - Behçet's disease - Polymyalgia rheumatica - Eosinophilic fasciitis - Hypermobility
Dorsopathies
Kyphosis - Lordosis - Scoliosis - Scheuermann's disease - Spondylolysis - Torticollis - Spondylolisthesis - Spondylopathies (Ankylosing spondylitis, Spondylosis, Spinal stenosis) - Schmorl's nodes - Degenerative disc disease - Coccydynia - Back pain (Radiculopathy, Neck pain, Sciatica, Low back pain)
Soft tissue disorders
muscle: Myositis - Myositis ossificans (Fibrodysplasia ossificans progressiva)
synovium and tendon: Synovitis/Tenosynovitis (Calcific tendinitis, Stenosing tenosynovitis, Trigger finger, DeQuervain's syndrome) - Irritable hip - Ganglion cyst
bursa: bursitis (Olecranon, Prepatellar, Trochanteric) - Baker's cyst
fibroblastic disorders (Dupuytren's contracture, Plantar fasciitis, Nodular fasciitis, Necrotizing fasciitis, Fasciitis, Fibromatosis)
shoulder lesions: Adhesive capsulitis - Rotator cuff tear - Subacromial bursitis
enthesis: enthesopathies (Iliotibial band syndrome, Achilles tendinitis, Patellar tendinitis, Golfer's elbow, Tennis elbow, Metatarsalgia, Bone spur, Tendinitis)other, NEC: Muscle weakness - Rheumatism - Myalgia - Neuralgia - Neuritis - Panniculitis - Fibromyalgia
Osteopathies
disorders of bone density and structure: Osteoporosis - Osteomalacia - continuity of bone (Pseudarthrosis, Stress fracture) - Monostotic fibrous dysplasia - Skeletal fluorosis - Aneurysmal bone cyst - Hyperostosis - OsteosclerosisOsteomyelitis - Avascular necrosis - Paget's disease of bone - Algoneurodystrophy - Osteolysis - Infantile cortical hyperostosis
Chondropathies
Juvenile osteochondrosis (Legg-Calvé-Perthes syndrome, Osgood-Schlatter disease, Köhler disease, Sever's disease) - Osteochondritis - Tietze's syndrome
See also congenital conditions (Q65-Q79, 754-756)
Retrieved from "http://en.wikipedia.org/wiki/Degenerative_disc_disease"
For information on another disease, please click on Digestive Diseases Library.
Digestive Diseases Library
2 comments:
It is nothing to worry about,though there doesn't seem to be a known cause or a known "cure".If you have any problems with toenail,it could also effect the sinus or even be a sign of unhealthy organs.
Did you look at our page on bunions treatment?
ebunionstreatment.com
As a sign of gratitude for how my husband was saved from Lymes, I decided to reach out to those still suffering from this.
My husband suffered from Lymes and it was really tough and heartbreaking for me because he was my all and the symptoms were terrible, we tried various therapies prescribed by our neurologist but none could cure him. I searched for a cure and I saw testimony of so many people who were cured from Lymes , and so many others with similar body problems, and they left the contact of this doctor who had the herbal cure to Lymes. I never imagined Lymes had a cure not until I contacted him and he assured me my husband will be fine. I got the herbal medication he recommended and my husband used it and in one months he was fully okay even up till this moment he is so full of life.Lymes has a cure and it is a herbal cure contact the doctor for more info on drituaherbalcenter@gmail.com Dr Itua can cure Herpes,Hiv,Cancer,ALS,Copd,HPV,Lupus,MS,Diabetes, and other disease talk to Dr Itua on how to get the medication. Thanks for reading my testimony .
Post a Comment